Anterior Cruciate Ligament Reconstruction: Graft Options and Rehabilitation Protocols
Introduction to Anterior Cruciate Ligament (ACL) Reconstruction
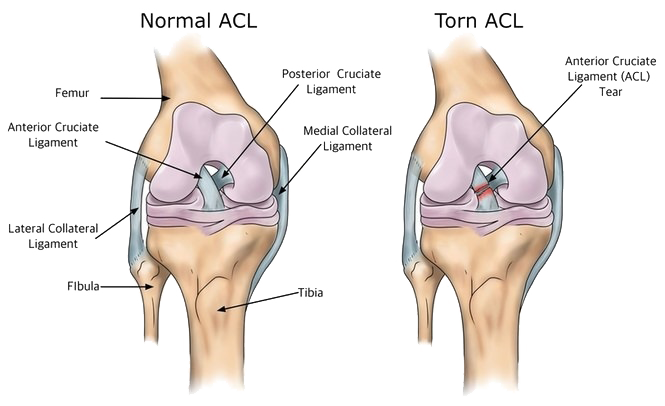
The anterior cruciate ligament (ACL) plays a critical role in maintaining the stability of the knee joint. This ligament connects the femur (thigh bone) to the tibia (shin bone), and it is essential for controlling movements such as walking, running, and jumping. When the ACL is injured, often through sports activities or trauma, it can lead to significant instability in the knee, which can severely impact a person’s mobility and quality of life.
A common cause of ACL injuries is sudden changes in direction or rapid deceleration during physical activities. Athletes participating in sports such as soccer, basketball, and skiing are particularly susceptible to these types of injuries. Additional risk factors include inadequate conditioning, improper footwear, and anatomical predispositions. Recognizing these factors is crucial for both prevention and necessary intervention.
When an ACL injury occurs, surgical reconstruction is often required, especially in young, active individuals. The significance of surgical intervention lies in restoring knee stability and enabling patients to return to their pre-injury activity levels. ACL reconstruction aims to replace the torn ligament with a graft, which can successfully restore function and stability to the knee joint.
Multiple graft options are available for ACL reconstruction, each with its own advantages and disadvantages. The most commonly used types of grafts include autografts, which are taken from the patient’s own body, and allografts, which are harvested from a deceased donor. Autografts often lead to faster healing and less risk of rejection, while allografts can reduce donor site morbidity. Selecting the appropriate graft is a critical component of the surgical process and can significantly influence the outcome of the surgery.
Types of Grafts for ACL Reconstruction
Anterior cruciate ligament (ACL) reconstruction is a common orthopedic procedure aimed at restoring knee stability following an ACL tear. A critical aspect of this surgery is the selection of an appropriate graft type. Grafts used in ACL reconstruction can be categorized into two main types: autografts and allografts. Each category has its own advantages and disadvantages, as well as specific indications that guide their use.
Autografts are harvested from the patient’s own body and commonly include the hamstring tendon and the patellar tendon. The hamstring tendon graft, often taken from the semitendinosus or gracilis muscle, is a popular choice due to its minimal donor site morbidity and good strength. This type of graft is beneficial for athletes seeking high levels of activity post-surgery. However, it may not be suitable for every patient, particularly those who may have compromised hamstring function or require extensive rehabilitation.
On the other hand, the patellar tendon graft is known for its robust structural integrity and has been widely utilized for years. This graft involves taking a strip of tendon from the knee cap, providing a strong fixation point. Though it is favored for its strength, it is associated with potential complications such as anterior knee pain and patellar issues, which may affect recovery. Surgeons often recommend this option for patients involved in high-impact sports.
In contrast, allografts are sourced from deceased donors and offer a convenient alternative, especially beneficial for older patients or those who wish to avoid additional surgical sites. While allografts eliminate the complications associated with harvesting tissue from the body, they are associated with a slightly increased risk of graft rejection and longer integration times. This results in variable outcomes compared to autografts, depending on the patient's lifestyle and rehabilitation commitment.
When selecting the appropriate graft type for ACL reconstruction, considerations such as age, activity level, and personal preferences play a vital role. By understanding the benefits and drawbacks associated with each option, both surgeons and patients can make informed decisions tailored to individual needs.
Comparative Analysis of Autografts and Allografts
The choice of graft type in anterior cruciate ligament (ACL) reconstruction significantly influences recovery outcomes. Autografts, which utilize tissue harvested from the patient’s own body, and allografts, sourced from a deceased donor, represent the primary options available for ACL repair. Each graft type presents unique advantages and disadvantages, specifically concerning recovery times, re-injury rates, and long-term functional outcomes.
Recovery times associated with autografts are often perceived to be more favorable due to the surgical technique and healing process. Studies indicate that patients receiving autografts generally return to their pre-injury levels of activity more quickly. However, the harvesting procedure can lead to additional postoperative pain and complications at the donor site, potentially affecting the recovery trajectory. Conversely, allografts eliminate the donor site morbidity but may be associated with a slightly longer recovery period as the graft integrates with the recipient's tissue.
Re-injury rates are another critical factor in graft selection. Research suggests that autografts may offer lower re-injury rates, particularly among younger athletes and those engaged in high-demand sports. Allografts, while effective, may present a higher risk of re-injury, especially if the graft does not integrate properly. Some studies advocate for the use of allografts in older patients or those with lower activity levels, as these patients may not require the high tensile strength provided by autografts.
Long-term outcomes also vary between these graft types. Autografts have consistently shown promising results over time, with many patients reporting satisfactory knee function. Allografts, however, can provide successful results as well, especially in individuals who are not involved in competitive sports. Ultimately, the choice between autografts and allografts should be tailored to the patient's specific needs, lifestyle, and recovery goals, ensuring optimal outcomes following ACL reconstruction.
Rehabilitation Protocols for Hamstring Tendon Grafts
Rehabilitation following anterior cruciate ligament (ACL) reconstruction using hamstring tendon grafts involves a structured approach aimed at restoring knee function and strength. The rehabilitation journey typically consists of several key stages: initial recovery, progressive strengthening, and return-to-sport phases. Each stage has specific goals, timelines, and exercises vital for optimal recovery.
Initially, after the surgical procedure, patients enter the recovery phase, which usually lasts from one to three weeks. Goals during this period focus on reducing swelling, managing pain, and restoring knee range of motion. Patients are often encouraged to perform gentle passive range-of-motion exercises, such as heel slides, alongside isometric quadriceps contractions. Additionally, modalities like ice and elevation play a crucial role in minimizing swelling. Crutches may be utilized to facilitate mobility while protecting the graft.
As patients progress to the strengthening phase, typically starting around three to six weeks post-surgery, the emphasis shifts towards enhancing muscle strength and stability around the knee. Exercises may include closed kinetic chain movements, such as mini squats and lunges, which are crucial for strengthening the quadriceps and hamstring muscles. Incorporating proprioceptive training, like balance exercises on unstable surfaces, is essential for regaining functional stability. This phase is integral in preparing for more dynamic activities.
Finally, the return-to-sport phase often commences at approximately six months post-operation, depending on individual progress and physician clearance. This critical stage involves sport-specific drills, agility training, and plyometric exercises to restore optimal athletic performance. Each rehabilitation protocol should be closely monitored and tailored to meet the individual’s unique needs, ensuring that they are physically and psychologically prepared to reintegrate into their sport safely.
Following these meticulously designed rehabilitation protocols not only enhances recovery after hamstring tendon graft reconstruction but also significantly reduces the risk of re-injury, supporting a successful return to pre-injury levels of activity.
Rehabilitation Protocols for Patellar Tendon Grafts
Rehabilitation following anterior cruciate ligament (ACL) reconstruction using patellar tendon grafts is a structured process designed to restore knee function and strength. The protocol is often divided into stages that progress from post-surgical care to more advanced functional training, ensuring a comprehensive recovery. Immediately after surgery, the focus is on managing pain and swelling. Ice, elevation, and appropriate medications play crucial roles in this initial stage.
As patients begin the rehabilitation journey, the first milestone typically includes achieving full knee extension and gradually regaining range of motion. A stable and controlled environment is vital during this phase, as it involves gentle passive and active exercises. For instance, straight leg raises and knee bends are commonly prescribed to initiate movement without compromising the graft's integrity.
Moving into the next phase, patients are introduced to weight-bearing exercises. Progressing from crutches to full weight-bearing is a critical step, allowing strengthened muscle engagement. Exercises may include improving quadriceps strength through isometric contractions and utilizing stationary bicycles or aquatic therapy for low-impact conditioning. It is during this stage that rehabilitation protocols for patellar tendon grafts show some divergence from hamstring tendon protocols, particularly in terms of the stress placed on the graft and the timeline for returning to sports. While both graft types emphasize rebuilding strength and mobility, patellar tendon rehabilitation often features more aggressive knee extension exercises due to its anatomical performance.
As patients advance towards functional training, agility drills and sports-specific movements become essential components of the rehabilitation program. Regular reassessments are crucial to monitor progress and make timely adjustments to the protocol. This multifaceted approach helps ensure a successful return to pre-injury levels of activity, emphasizing patient safety and graft stability throughout the rehabilitation journey.
Rehabilitation Protocols for Allografts
Rehabilitation following anterior cruciate ligament (ACL) reconstruction using allografts necessitates a tailored approach due to unique considerations related to graft integration and individual patient factors. Unlike autograft procedures, where the ligament is derived from the patient’s own tissue, allografts are sourced from donor tissue, which can impact healing times and the rehabilitation timeline. The primary objective during this rehabilitation phase is to ensure optimal graft integration while minimizing the risk of re-injury.
Initially, rehabilitation begins with a focus on controlling pain and swelling, which is crucial for the healing process. Cryotherapy and compression techniques may be utilized to manage inflammation effectively. Early range of motion exercises are introduced to prevent stiffness and enhance mobility, carefully monitored to avoid excessive strain on the newly implanted graft. The rehabilitation protocol will typically emphasize gradual progression through different phases, each addressing specific goals that align with the healing stages of the allograft tissue.
As the early phase progresses, emphasis shifts towards strengthening exercises that target the quadriceps and hamstring muscles, which provide stability to the knee joint. Exercise regimens are designed to adapt based on patient-specific dynamics, incorporating functional activities as tolerated. It is essential to educate patients on the importance of adhering to the prescribed rehabilitation plan, as individual compliance significantly influences recovery outcomes.
One crucial aspect specific to allograft rehabilitation is monitoring the integration process. Physiotherapists may utilize various assessments to gauge the progress of the graft incorporation into the host tissue. Individual factors such as age, activity level, and the type of rehabilitation undertaken alongside allograft considerations play a critical role in tailoring recovery protocols, ultimately aiming for a successful return to pre-injury activity levels.
Conclusion and Future Directions in ACL Reconstruction
In the realm of anterior cruciate ligament (ACL) reconstruction, various graft options along with tailored rehabilitation protocols play a crucial role in optimizing patient recovery and overall outcomes. The necessity of individualized graft selection cannot be overstated, as it must cater to each patient's unique anatomical and physiological characteristics, along with their lifestyle and activity levels. The synthesis of patient-specific needs and the surgeon's expertise is pivotal for achieving successful surgical interventions.
Throughout this discussion, we have highlighted the significance of understanding different types of grafts, including autografts and allografts, along with their respective advantages and disadvantages. The choice of graft has profound implications not only on surgical success but also on the subsequent rehabilitation process, which is essential for a return to pre-injury function. Comprehensive rehabilitation protocols, which incorporate strength training, neuromuscular re-education, and functional tasks, contribute significantly to the long-term stability of the knee. They also play a vital role in mitigating the risk of re-injury.
Looking ahead, the future of ACL reconstruction research is promising. Innovations in graft technology, such as bioengineered grafts, present new opportunities that may enhance graft integration and overall recovery. Furthermore, advancements in rehabilitation methodologies, including virtual reality and personalized training programs, are paving the way for improved healing experiences. Such technologies can help validate the effectiveness of rehabilitation protocols and tailor them according to individual progress.
As medical professionals continue to explore these advancements, the core goal remains the same: to enhance patient outcomes post-ACL surgery. Ongoing research, clinical trials, and collaborative efforts among professionals in the field will ultimately lead to refined surgical techniques and rehabilitation practices, benefiting those who undergo this common yet critical orthopedic procedure.
