Shoulder Arthroscopy
SHOULDER
What is Shoulder Arthroscopy?
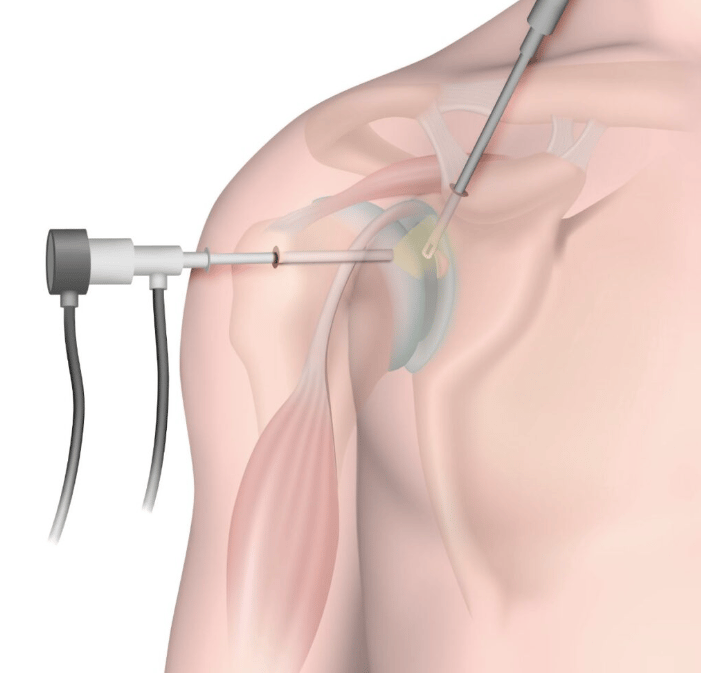
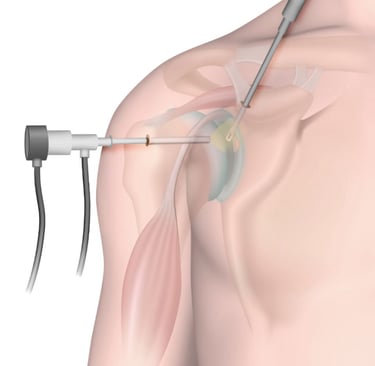
Shoulder arthroscopy is a minimally invasive surgical procedure that enables orthopedic surgeons to visualize, diagnose, and treat various shoulder disorders with enhanced precision. Utilizing advanced technology, this technique involves inserting a small camera, known as an arthroscope, through tiny incisions in the skin. This camera captures high-definition images of the shoulder joint, allowing physicians to assess the condition of the soft tissues, cartilage, and bones within the joint space.
The instruments used during shoulder arthroscopy are specialized tools designed to manipulate tissues without causing significant damage to the surrounding areas. This is beneficial in reducing recovery times and minimizing post-operative pain when compared to traditional open surgery. The advancement of arthroscopic technology has revolutionized the treatment of several shoulder ailments, such as rotator cuff tears, impingement syndromes, and adhesive capsulitis (frozen shoulder).
Historically, shoulder arthroscopy has evolved since its inception in the 20th century, expanding the possibilities for effective treatment of shoulder conditions. The procedure has gained popularity due to its minimally invasive nature, which typically results in less scarring and quicker rehabilitation. Over the years, advancements in imaging and surgical techniques have improved the surgeon's ability to address complex conditions. Additionally, with the introduction of 3D imaging and enhanced visualization tools, shoulder arthroscopy is continually becoming more refined.
This surgical approach is particularly advantageous for patients, as it not only provides an effective means of intervention but also encourages a faster return to daily activities and sports. As the technique continues to progress, patients can expect further improvements in outcomes and overall satisfaction from shoulder arthroscopy procedures.
Indications for Shoulder Arthroscopy
Shoulder arthroscopy is a minimally invasive surgical procedure frequently utilized to address various shoulder conditions. One primary indication for this procedure is a rotator cuff tear, which can cause significant pain and weakness, affecting daily activities and overall quality of life. Such tears often result from age-related degeneration or acute injuries, leading to compromised shoulder function. The symptoms typically include persistent shoulder pain, decreased range of motion, and difficulty with overhead movements.
Another condition that commonly necessitates shoulder arthroscopy is impingement syndrome. This occurs when the rotator cuff tendons are compressed during shoulder movements, resulting in pain, particularly when lifting the arm. Patients may experience aching discomfort, stiffness, and referred pain, which can severely limit their range of motion and participation in physical activities.
Shoulder instability is an additional indication that may warrant the use of arthroscopy. This condition involves excessive motion of the shoulder joint, potentially leading to recurrent dislocations. Individuals suffering from shoulder instability often report episodes of the shoulder 'giving way,' along with pain and the fear of re-injury, which can markedly diminish their ability to engage in sports and other physical pursuits.
Lastly, labral tears, which involve damage to the cartilage that stabilizes the shoulder joint, are also prevalent reasons for recommending shoulder arthroscopy. These injuries can result from trauma or repetitive motion, manifesting as a catching sensation or popping noises within the joint, accompanied by pain and reduced range of motion. As these conditions impact the overall functionality of the shoulder, timely intervention through arthroscopy can significantly enhance patient outcomes, allowing for a return to everyday activities and improved quality of life.
Preparing for Shoulder Arthroscopy
Preparing for shoulder arthroscopy is a crucial step in ensuring a successful surgical outcome. Patients must complete several essential tasks prior to the procedure. Firstly, a thorough pre-operative assessment will be conducted by the surgical team, which typically includes a comprehensive medical history review and a physical examination. This assessment helps to identify any risk factors that may complicate the surgery or recovery.
Engaging in open discussions with the surgical team is vital. Patients should not hesitate to ask about the procedure, potential risks, and expected outcomes. This conversation can also include clarification regarding anesthesia options and post-operative care. Understanding these aspects can alleviate anxiety and foster a sense of collaboration between the patient and the healthcare team.
In addition to discussions with healthcare providers, certain medical tests may be required before the surgery. Common tests include blood work, imaging studies, and assessments of heart and lung function. These tests aid in evaluating the patient's overall health and contribute to the surgical team's preparedness, ensuring that any underlying issues are addressed prior to the procedure.
Furthermore, lifestyle adjustments may be necessary in the days leading up to the surgery. Patients are typically advised to avoid certain medications, especially blood thinners, which can increase the risk of bleeding during and after the surgery. It is critical for patients to inform their healthcare providers of all medications they are currently taking, including over-the-counter drugs and supplements.
Additionally, patients should be prepared to make arrangements for post-operative care, including having someone available to assist with daily activities as mobility may be limited during the initial recovery phase. By taking these preparatory steps seriously, patients enhance the likelihood of a successful shoulder arthroscopy and a smoother recovery process.
The Shoulder Arthroscopy Procedure
Shoulder arthroscopy is a minimally invasive surgical procedure that utilizes small incisions to access the interior of the shoulder joint. The procedure typically begins with the administration of anesthesia to ensure patient comfort. Options for anesthesia include general anesthesia, where the patient is fully asleep, or regional anesthesia, which numbs the shoulder area while the patient remains awake. The choice of anesthesia largely depends on the extent of the surgery and the patient's medical history.
Once the anesthesia takes effect, the surgeon prepares the shoulder by making small incisions, usually one to three, through which a slender tube equipped with a camera, known as an arthroscope, is inserted. This arthroscope provides a live video feed of the shoulder joint, allowing the surgeon to examine structures such as the rotator cuff, labrum, and bursa for any abnormalities or damage.
Following the examination, the surgeon may proceed with any necessary repairs or interventions. This can include smoothing out frayed cartilage, repairing tears in the rotator cuff, or removing loose debris from the joint. Specialized instruments are typically inserted through the additional incisions to facilitate these repairs. The total duration of the procedure can vary, generally lasting between 30 minutes to two hours, depending on the complexity of the intervention.
The surgical team plays a critical role in ensuring the smooth execution of the procedure. A skilled surgeon leads the operation, while anesthesiologists monitor the patient’s vital signs throughout the process, ensuring optimal safety. Additionally, surgical nurses assist in maintaining a sterile environment and providing support to the surgeon. Overall, shoulder arthroscopy is designed to minimize recovery time while addressing various shoulder issues effectively. The use of advanced arthroscopic techniques generally results in less postoperative pain and quicker rehabilitation, giving patients a favorable outcome.
Post-Operative Care and Rehabilitation
Post-operative care following shoulder arthroscopy is critical for ensuring a successful recovery and enhancing the patient's overall outcome. Initially, patients can expect a recovery period that may vary from person to person, typically lasting a few weeks. During this time, rest is paramount, but patients are also encouraged to follow their surgeon's specific protocols to promote healing effectively.
Pain management is a vital aspect of recovery. Most patients experience some level of discomfort post-surgery, which may be alleviated using prescribed analgesics or over-the-counter medications, as recommended. Ice therapy can also help reduce swelling and relieve pain during the initial recovery phase. It is essential for patients to communicate any persistent or severe pain to their healthcare provider, as this may indicate complications requiring further evaluation.
Following the acute recovery phase, engaging in a structured rehabilitation program becomes essential. Physical therapy often starts shortly after the surgery, typically under the guidance of a licensed therapist with experience in shoulder rehabilitation. The rehabilitation protocol emphasizes gradual progression. Initially, the focus is on gentle range-of-motion exercises that aim to restore mobility without straining the surgical site.
As patients advance in their rehabilitation, strength training and functional exercises become crucial. The timeline for returning to normal activities, including sports or heavy lifting, largely depends on individual healing rates and adherence to the rehabilitation protocol. Most patients can expect to resume light activities approximately six weeks after surgery, with a gradual return to more intense activities taking longer, potentially several months.
Monitoring for potential complications, such as increased pain, swelling, or signs of infection, should remain a priority throughout the recovery process. Regular follow-up appointments with the healthcare provider are crucial for assessing progress and making any necessary adjustments to the rehabilitation plan, ultimately leading to a successful return to daily activities.
Potential Risks and Complications
Shoulder arthroscopy, while recognized for its minimally invasive nature, is not devoid of potential risks and complications that patients should be aware of prior to undergoing the procedure. Understanding these risks enhances informed consent and prepares patients for the postoperative journey.
One of the primary concerns is the risk of infection. Although the incidence of infection in arthroscopic procedures is relatively low, it remains a possibility. Keeping the surgical site clean and following the post-operative care instructions provided by the surgeon can significantly reduce this risk. If any signs of infection, such as increased redness, swelling, or discharge are observed, it is imperative to contact a healthcare provider promptly.
Nerve damage is another potential complication, as nearby nerves may be injured during the procedure. While instances of nerve damage are uncommon, they can lead to numbness, tingling, or weakness in the arm or shoulder. Most nerve injuries are temporary; however, in rare cases, they may result in long-lasting effects. Patients are encouraged to discuss the specific risks with their surgeon and understand the baseline function of their nerves before surgery.
Stiffness is a common post-operative concern, particularly in the initial rehabilitation phase. Patients may experience reduced range of motion as the shoulder heals. Engaging in recommended physical therapy is vital for addressing stiffness and ensuring optimal recovery. Therapy can help restore mobility while also strengthening the surrounding muscles, which contributes to overall shoulder function.
Finally, there is a possibility of recurrence of shoulder issues, particularly if the underlying causes are not adequately addressed. Patients should engage actively in their rehabilitation and heed the surgeon’s advice on activity modifications to minimize the chances of re-injury. By understanding these risks and adhering to post-operative guidelines, patients can better navigate the recovery process following shoulder arthroscopy.
Patient Success Stories and Experience
Shoulder arthroscopy has emerged as a leading choice for individuals suffering from various shoulder conditions, and the success stories of previous patients serve as a testament to its effectiveness. Many individuals have reported significant improvements in their shoulder function, mobility, and overall quality of life following the procedure. For example, a 55-year-old patient who underwent shoulder arthroscopy for a rotator cuff tear shared their experience of immediate relief from chronic pain and the ability to return to regular activities just a few months post-surgery. Such testimonials highlight the transformative impact of the procedure.
Moreover, patient experiences often encompass not only physical improvements but also emotional and psychological gains. Many individuals express feelings of renewed hope and empowerment after seeing substantial progress in their rehabilitation process. A patient recovering from a shoulder impingement stated that the emotional burden of persistent pain was alleviated, allowing them to engage more actively with family and friends again. This aspect of recovery underscores the holistic benefits that shoulder arthroscopy can provide, beyond mere physical outcomes.
Research and statistics further back these personal stories with concrete evidence of surgery effectiveness. Studies indicate that the success rates of shoulder arthroscopy are remarkably high, with approximately 80-90% of patients reporting satisfactory results. Additionally, patients typically describe decreased pain levels and improved functional outcomes, especially when adhering to prescribed rehabilitation programs. Such data not only emphasize the technical proficiency of shoulder arthroscopy but also foster a sense of reassurance for those contemplating surgery.
In essence, the amalgamation of patient testimonials, emotional experiences, and solid research findings collectively builds confidence and encourages individuals facing shoulder issues to consider shoulder arthroscopy as a viable treatment option.
