Shoulder Instability
SHOULDER
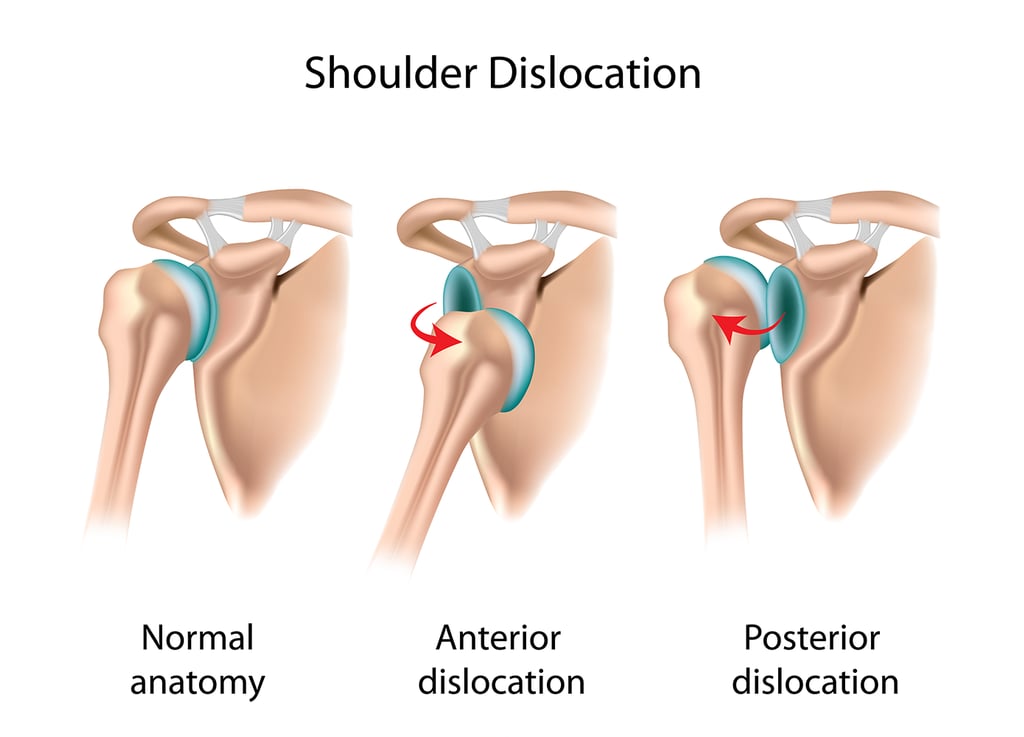
Shoulder instability is a condition where the shoulder joint experiences excessive motion, potentially leading to dislocations, subluxations, or chronic pain. This instability can arise from acute trauma, repetitive stress, or anatomical abnormalities. This condition can lead to significant disability for an individual affecting his daily activities of life.
Effective management is crucial to restore joint function and prevent recurrence. There has been more awareness and advancements in treatment approaches reflect a deeper understanding of the condition’s pathophysiology and improved technological capabilities.
How do we assess?
History:
Pain, Weakness, or feelings of the shoulder “giving way.” History of dislocations, subluxations (partial dislocations), or trauma.
Activity Level: Understand the patient's activity level and any specific movements that exacerbate symptoms.
Past treatments: Inquire about past treatments, including physical therapy or surgeries.
Physical Examination:
Range of Motion and Rotator cuff Testing
Apprehension Test: For anterior instability, the shoulder is put in abduction and external rotation. A positive test is when the patient feels apprehensive or uncomfortable.
Relocation Test: After a positive apprehension test, applying posterior pressure to the shoulder can alleviate the apprehension.
Imaging Studies:
X-rays: Useful for assessing bone structures and detecting dislocations or fractures.
MRI or MR Arthrogram: Provides detailed images of soft tissues, including the labrum and rotator cuff tendons. An MR arthrogram, where contrast dye is injected into the shoulder joint, can better visualize labral tears.
CT Scan: Sometimes used to evaluate bone loss.
Ultrasound:
Helps evaluate soft tissues, such as the rotator cuff and labrum, particularly if MRI is contraindicated.
Dynamic Ultrasound can be used to visualize real-time shoulder movement and assess instability during dynamic activities.
3D models and Simulation
Recent advancements in 3D imaging and simulation technologies have improved preoperative planning and surgical outcomes.
Artificial Intelligence and Machine Learning
Artificial intelligence (AI) and machine learning are increasingly being integrated into the management of shoulder instability.
Predictive Analytics: AI algorithms can analyze large datasets to predict patient outcomes and guide treatment decisions.
AI-based decision support systems assist clinicians in selecting the most appropriate treatment options based on patient-specific data.
How do we manage ?
A. Non-Surgical Management
1. Activity Modification and Education
2. Rehabilitation Protocols
Rehabilitation remains a cornerstone of non-surgical management for shoulder instability. It is important to personalize the rehabilitation protocols, tailored to the specific type and severity of instability in a patient.
Early Proprioceptive Training
Strengthening and Conditioning
Eccentric strengthening exercises targeting the rotator cuff and scapular stabilizers
Neuromuscular Re-education including functional training and sport-specific drills, are increasingly used to restore dynamic stability
Physiotherapy rehabilitation after surgical treatment
B. Surgical Management
Arthroscopic Techniques
Arthroscopic surgery has revolutionized the management of shoulder instability, offering less invasive options with improved recovery profiles. Recent advancements in arthroscopic techniques have enhanced repair precision and durability.
Bankart Repair
The Bankart repair involves arthroscopically repairing the glenoid labrum.
Remplissage procedure is often combined with Bankart repair for patients with engaging Hill-Sachs lesions, which are defects on the posterior aspect of the humeral head. Remplissage involves filling the Hill-Sachs lesion with a portion of the infraspinatus tendon to prevent recurrent instability.
Latarjet Procedure
The Latarjet procedure, involving the transfer of the coracoid process to the glenoid, remains a viable option for patients with severe instability. Recent modifications to this technique, including improved fixation methods and the use of biologic agents, have led to better outcomes.
Biological Augmentation
Biological augmentation techniques aim to enhance tissue healing and improve surgical outcomes. Recent studies have explored the use of platelet-rich plasma (PRP) and stem cell therapies in shoulder instability management.
Platelet-Rich Plasma (PRP) therapy involves the injection of concentrated platelets into the surgical site to promote tissue healing. Stem cell therapy, utilizing adipose-derived or bone marrow-derived stem cells, has shown promise in enhancing tendon and cartilage repair.
Modern Suture Anchors
The design and material of suture anchors have evolved to enhance fixation strength and minimize complications. Nguyen et al. (2024) highlighted that newer suture anchor designs provided superior anchor pull-out strength and reduced the incidence of hardware-related complications.
Biodegradable Implants
The introduction of biodegradable implants has reduced the need for hardware removal and decreased postoperative pain.
All suture implants
These recent implants minimises bone disruption by allowing for smaller drill holes and stronger fixation in osteoporotic bones.
The management of shoulder instability involves a multifaceted approach that includes accurate diagnosis, conservative treatment, and surgical interventions. Advances in surgical techniques and rehabilitation protocols continue to improve outcomes for patients with shoulder instability.