Total Shoulder Replacement: Anatomic and Reverse Shoulder Replacement
SHOULDER
Introduction to Shoulder Replacement
Shoulder replacement surgery is a significant medical procedure aimed at alleviating pain and restoring functionality in patients suffering from severe shoulder conditions. The primary purpose of this intervention is to replace damaged or arthritic components of the shoulder joint with artificial implants, thus providing relief and improving the quality of life. Conditions often treated by this procedure include osteoarthritis, rheumatoid arthritis, and significant rotator cuff tears, all of which cause pain, stiffness, and functional limitations.
The shoulder joint is a complex anatomical structure composed of three major bones: the humerus, the scapula, and the clavicle. The interaction of these bones, along with tendons, ligaments, and muscles, enables a wide range of motion. The glenohumeral joint, formed by the humeral head and the glenoid cavity of the scapula, allows for the arm's extensive movement. However, trauma or degenerative diseases can severely compromise this joint’s integrity, necessitating surgical intervention.
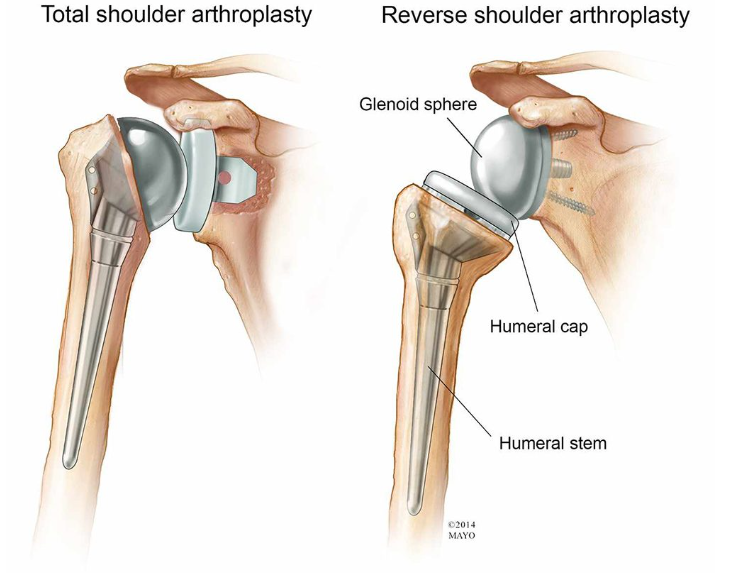
There are two primary types of shoulder replacements: anatomic and reverse. Anatomic shoulder replacement mirrors the shoulder's natural structure, while reverse shoulder replacement alters the joint mechanics to benefit patients with severe rotator cuff damage. The rationale for choosing either procedure often hinges on the patient’s specific condition, their anatomical needs, and overall health. As populations age and physical activity levels change, there has been a noticeable increase in the prevalence of shoulder replacements within orthopedic surgery practices. This rise reflects advancements in surgical techniques and artificial implant technologies, providing new options for those suffering from debilitating shoulder ailments.
Types of Shoulder Replacement: Anatomic vs. Reverse
Shoulder replacement surgery has evolved significantly over the years, leading to the development of two primary types of procedures: anatomic shoulder replacement and reverse shoulder replacement. Each of these approaches is designed to address specific conditions affecting the shoulder joint, and their distinct characteristics warrant careful consideration when evaluating treatment options.
Anatomic shoulder replacement, often utilized for patients with arthritis or trauma affecting the glenohumeral joint, involves replacing the damaged portions of the shoulder with implants that closely mimic the natural anatomy. The procedure typically utilizes a ball-and-socket implant system, wherein the humeral head is replaced with a prosthetic ball, while the socket (the glenoid) is lined with a polyethylene implant. The surgical technique requires precise alignment to ensure optimal shoulder mechanics, which allows for a more natural range of motion post-operation.
Conversely, reverse shoulder replacement is primarily indicated for patients with rotator cuff deficiency, severe arthritis, or failed prior shoulder surgeries. This procedure involves an inversion of the traditional implant design—here, the ball is attached to the shoulder socket, and a concave socket is placed on the upper arm bone (humerus). The reverse configuration redistributes the forces around the shoulder joint and employs different muscular dynamics, thus compensating for the lack of functional rotator cuff muscles. The surgical technique also necessitates careful consideration of patient anatomy, as the procedure aims to provide stability and improved range of motion in the affected joint.
In summary, anatomic and reverse shoulder replacements serve different patient needs and conditions, with variations in implant design and surgical techniques. Understanding these differences is crucial for patients and healthcare providers when deciding on the most appropriate intervention for shoulder pathologies.
Indications for Shoulder Replacement
Shoulder replacement surgery is often considered when conservative treatments, such as physical therapy, medications, and corticosteroid injections, have failed to alleviate debilitating pain or restore functionality. Several conditions can lead to the necessity for shoulder replacement, each impairing the joint's mechanics and causing significant discomfort.
One prevalent indication is severe osteoarthritis, a degenerative joint disease that results from the wear and tear of cartilage. This condition often causes joint stiffness, swelling, and pain during movement, ultimately making daily activities challenging. When the damage is extensive and pain becomes chronic, shoulder replacement may become the most viable option for restoring the patient’s quality of life.
Rheumatoid arthritis, an autoimmune disorder, is another critical consideration for shoulder replacement. This condition leads to inflammation of the joints, resulting in pain, stiffness, and potential joint deformity. As the disease progresses, it can severely limit shoulder mobility. Surgical intervention aims to alleviate pain and improve function in those where joint preservation techniques have been exhausted.
Rotator cuff tear arthropathy, which combines a significant rotator cuff tear with arthritis, can also necessitate shoulder replacement. The rotator cuff plays a crucial role in stabilizing the shoulder; however, when torn and combined with arthritic changes, patients may experience debilitating pain and loss of motion. In such cases, shoulder replacement may be required to replace both the damaged joint surface and address the functional deficits caused by rotator cuff failure.
Lastly, post-traumatic arthritis, which can occur after a shoulder fracture or injury, presents another reason for surgical consideration. Damage incurred from trauma can lead to joint instability, significant pain, and the development of arthritis over time. When non-surgical treatments prove ineffective, shoulder replacement can restore mobility and relieve the suffering caused by this condition.
The Surgical Procedure: What to Expect
Before undergoing a shoulder replacement, whether anatomic or reverse, patients will typically participate in a comprehensive preoperative assessment. This assessment may include imaging tests such as X-rays or MRIs, as well as blood tests to evaluate overall health. The orthopedic surgeon will discuss the patient’s medical history, current medications, and any potential risks associated with the surgery. It is also vital for patients to communicate any concerns they might have prior to the operation.
For pain management during the procedure, general anesthesia is commonly employed. Under general anesthesia, the patient is fully unconscious and will not experience any discomfort throughout the surgery. In some cases, regional anesthesia may be utilized, which numbs the shoulder area but keeps the patient awake. The choice of anesthesia will depend on the individual patient’s circumstances and surgeon preference.
The surgical approach will vary depending on whether the procedure is an anatomic or reverse shoulder replacement. Typically, the orthopedic surgeon will make an incision on the front of the shoulder, measuring about 6 to 8 inches in length. This incision provides access to the shoulder joint. During an anatomic shoulder replacement, the damaged components of the joint are removed and replaced with prosthetic components that mimic the natural anatomy. Conversely, in a reverse shoulder replacement, the surgeon will alter the mechanics of the shoulder by placing the ball component on the shoulder blade and the socket on the upper arm bone. Both procedures aim to relieve pain and restore function to the shoulder.
Throughout the procedure, a dedicated surgical team, consisting of the orthopedic surgeon, surgical assistants, anesthesiologists, and nursing staff, work meticulously to ensure patient safety and surgical effectiveness. Their expertise is crucial in navigating the complexities of the operation, leading to better outcomes and recovery for the patient.
Recovery and Rehabilitation Post-Surgery
Following shoulder replacement surgery, whether anatomic or reverse, patients typically experience a recovery period that varies in duration and intensity depending on various factors such as age, overall health, and the complexity of the surgery. The initial phase of recovery primarily occurs within the first few weeks, often characterized by swelling, discomfort, and limited mobility in the affected arm. It is essential for patients to adhere to their physician's guidelines during this critical phase to optimize healing and minimize complications.
Immediately post-surgery, pain management is a crucial aspect of recovery. Physicians often prescribe analgesics or recommend over-the-counter pain relievers to help alleviate discomfort. Additionally, applying ice packs to the shoulder can provide relief and reduce inflammation. It is important for patients to communicate openly with their healthcare providers regarding pain levels and any adverse reactions to medications. Adjustments may be necessary based on these discussions to ensure a more comfortable recovery experience.
Physical therapy plays a significant role in the rehabilitation process following shoulder replacement. Once cleared by the healthcare team, patients typically begin a structured physical therapy program to regain strength, flexibility, and function in the shoulder. This program often includes specific exercises aimed at restoring range of motion, alongside guidance on safe techniques for performing daily activities. Early mobilization is generally encouraged, but high-impact activities and sports should be approached cautiously and introduced gradually, ideally under the supervision of a qualified physical therapist.
During the recovery timeline, it is also vital for patients to monitor for potential complications, such as signs of infection, persistent swelling, or unusual pain that may indicate issues such as joint instability. Early detection of these complications can significantly impact the overall recovery trajectory. Following a steady progress marked by achieving common recovery milestones, patients can look forward to a return to their regular activities and, eventually, sports, reinforcing the importance of patience and persistence throughout the rehabilitation journey.
Potential Risks and Complications
Shoulder replacement surgery, whether anatomic or reverse, is typically performed to relieve pain and restore function in individuals with severe shoulder joint damage. While the procedure has a high success rate, like any surgical intervention, it carries potential risks and complications that patients should carefully consider.
One of the most common general surgical risks includes infection. Although the incidence of infection following shoulder replacement is relatively low, it can lead to severe complications if not properly addressed. Patients are usually given prophylactic antibiotics before and after surgery to minimize this risk. Another potential concern is bleeding, which may occur during or after the procedure and could necessitate a blood transfusion in rare cases.
Specific complications related to the shoulder itself include implant failure and stiffness. Implant failure can occur if the prosthetic components loosen, resulting in pain or decreased functionality. Stiffness, or decreased range of motion, may arise post-surgery, often resulting from scarring or the natural healing process. Patients may require physical therapy to help regain mobility and strength, emphasizing the importance of postoperative rehabilitation.
Additionally, nerve damage is a potential risk associated with shoulder replacement surgery. Nerve injuries can lead to weakness, numbness, or pain in the arm, and they may be temporary or, in some instances, permanent. It is essential for patients to discuss these risks thoroughly with their orthopedic surgeon, as well as the specific factors that might increase their susceptibility to complications, such as age, health status, and previous surgeries.
Despite these risks, it is important to weigh them against the significant benefits that shoulder replacement can provide. Many patients experience substantial pain relief and improved function, often resulting in a better quality of life.
Patient Information and Resources
For individuals contemplating shoulder replacement surgery, it is crucial to arm oneself with the right information and resources. Preparing for surgery involves not only understanding the procedure but also equipping oneself with practical insights on pre-surgical preparation and recovery. Here are essential tips and resources that can aid patients in their journey.
First, patients should focus on their pre-surgical preparation. Prior to the surgery, it is advisable to maintain healthy habits, such as engaging in physical therapy to strengthen the shoulder muscles. Patients should also ensure they have a clear understanding of their medical history and any medications they are taking, as this information is vital for the surgical team. Creating a comfortable recovery environment at home, including arranging for assistance during the initial healing period, can significantly enhance the recovery experience.
Asking pertinent questions is also a fundamental part of the patient journey. Individuals should consider asking their surgeon about the specific type of shoulder replacement being proposed—anatomic or reverse—and the rationale behind this choice. Inquiries regarding the expected recovery timeline, potential risks, and follow-up rehabilitation plans are equally important. Patients might also want to discuss the surgeon’s experience, success rates, and what to expect during post-operative care.
Moreover, connecting with support groups and online forums can further empower patients by providing a platform for shared experiences. Websites like the American Academy of Orthopaedic Surgeons (AAOS) and the Arthritis Foundation offer valuable resources and provide avenues to connect with other patients who have undergone similar procedures. Recommended reading materials, such as “The Patient’s Guide to Shoulder Replacement Surgery,” can also provide deeper insights into surgical options and expectations.
By gathering knowledge and establishing a supportive network, patients can navigate their shoulder replacement journey with greater confidence and awareness.


